Understanding Shoulder Instability:
Dislocations, Labral Injuries, and Advanced Surgical Solutions
-
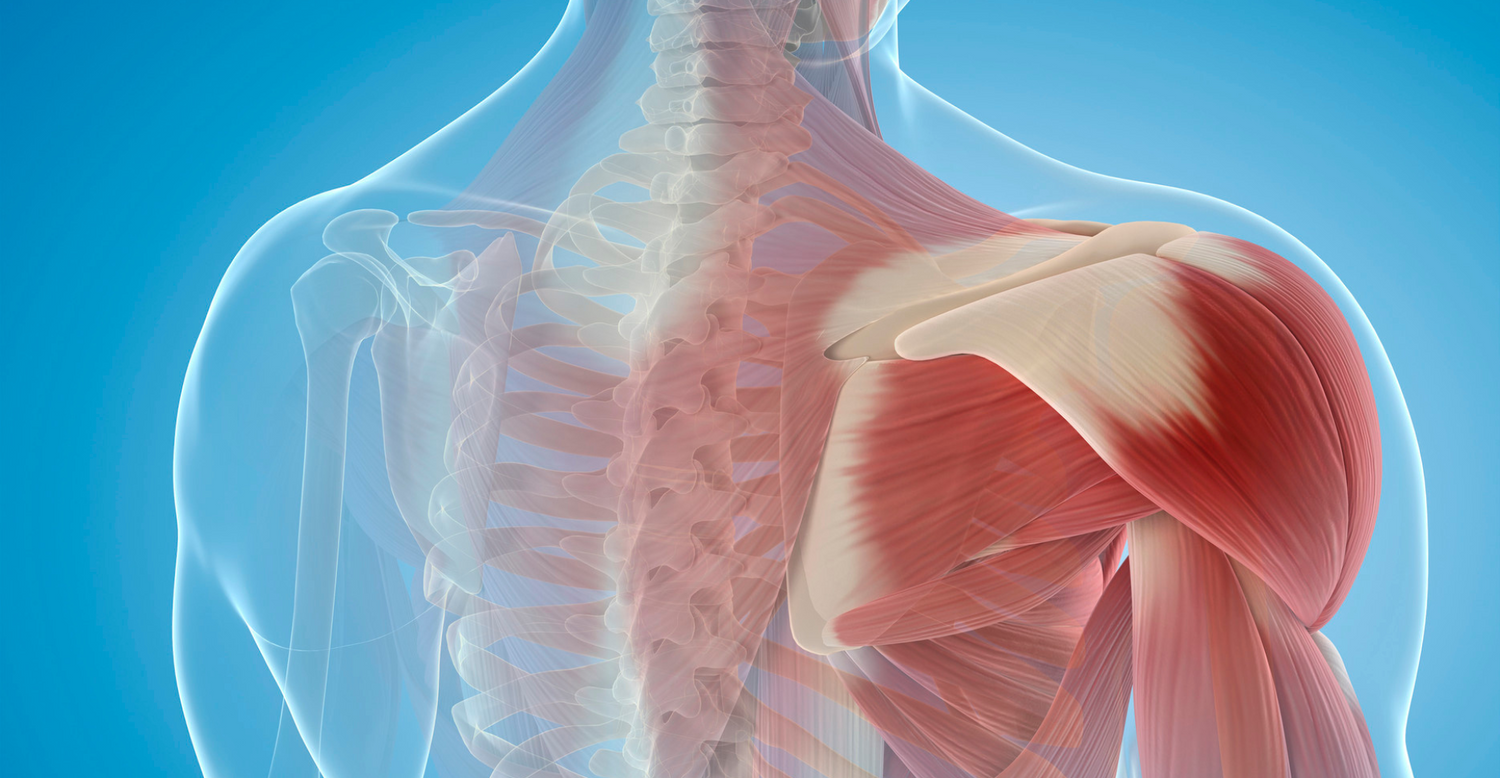
What Is Shoulder Instability?
Shoulder instability is a common orthopedic condition that occurs when the head of the humerus (upper arm bone) slips out of the glenoid (shoulder socket). This often results from a traumatic injury—frequently seen in contact sports or falls—and can lead to recurrent dislocations, labral tears, pain, weakness, and limited function.
-
It Most Commonly Affects:
The shoulder is the most mobile joint in the body, but this mobility comes at the cost of stability. When the soft tissues that hold the shoulder in place—particularly the labrum and capsule—are damaged, the shoulder can become unstable. Patients may experience:
- A sensation of the shoulder "slipping out"
- Recurrent dislocations or subluxations (partial dislocations)
- Pain during activity or overhead movement
- Decreased strength and range of motion
Apprehension or fear of dislocation during certain movements
Diagnosis and Expertise
Dr. Reza Jazayeri has extensive experience managing shoulder instability, from first-time dislocators to athletes with recurrent instability.
-

Labral Injury and the Bankart Lesion
A Bankart lesion refers to a tear of the anterior-inferior labrum, a ring of cartilage that deepens the shoulder socket and contributes to joint stability. This type of labral tear is commonly seen after a traumatic anterior shoulder dislocation.
Without appropriate treatment, a torn labrum can lead to chronic instability and higher risk of repeat dislocations—especially in young, athletic individuals.
-
The diagnostic process includes:
- A detailed clinical history and physical examination
- Advanced imaging (MRI with arthrogram and/or CT scan) to assess the labrum, capsule, and bone loss
- Functional assessment, especially in in-season athletes and overhead athletes
Dr. Jazayeri is nationally recognized for his expertise in treating shoulder instability. He has:
- Presented numerous lectures and research at major orthopedic conferences
- Led training sessions and cadaver labs on shoulder arthroscopy for residents and fellows
- Focused his academic discussions on return-to-play strategies for in-season athletes after traumatic dislocations
Dr. Jazayeri’s Surgical Approach:
Arthroscopic Bankart Repair with Advanced Techniques
-
What is Arthroscopic Bankart Repair?
Watch This VideoArthroscopic Bankart repair is a minimally invasive procedure performed using small incisions and a camera to reattach the torn labrum and tighten the capsule. Anchors with sutures are placed into the glenoid to secure the labrum and restore stability.
-
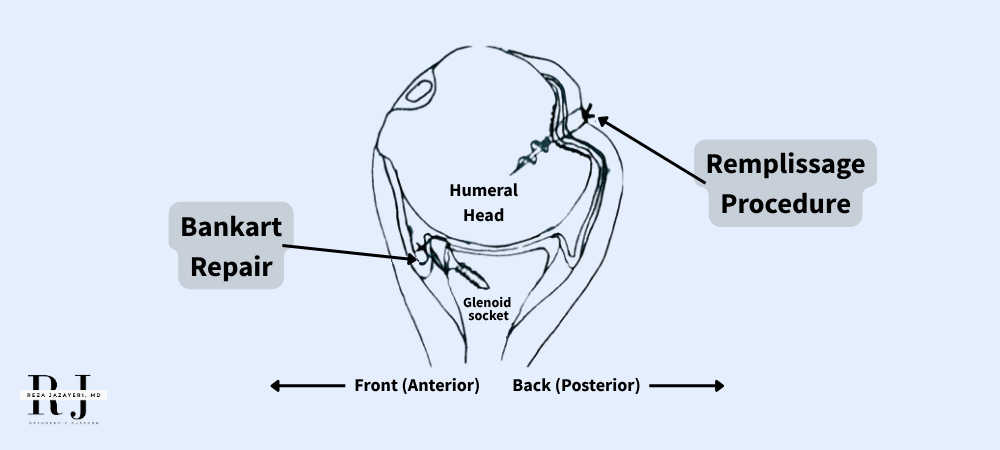
What Is the Remplissage Procedure?
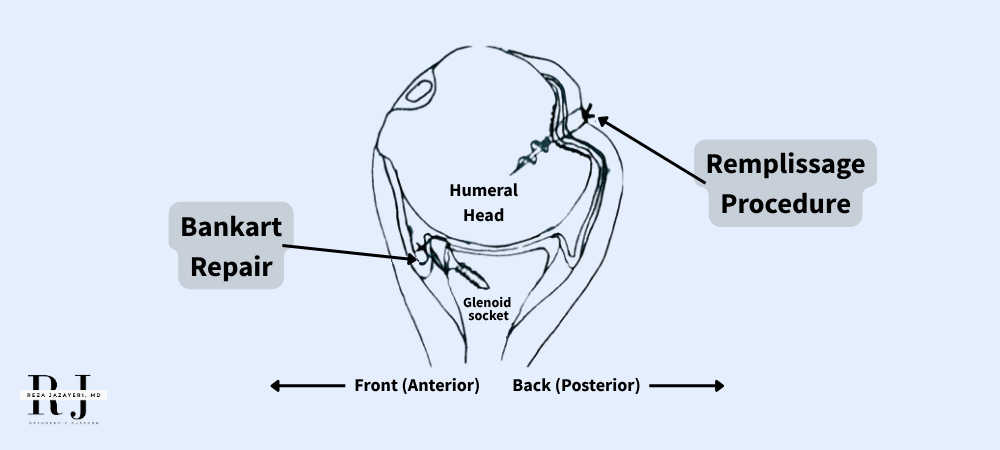
In patients with engaging Hill-Sachs lesions—a compression injury to the humeral head that occurs during dislocation—Dr. Jazayeri often incorporates a procedure called remplissage (French for "filling in").
The remplissage procedure involves anchoring the infraspinatus tendon into the Hill-Sachs defect, converting it into a non-engaging lesion. This "fills in" the bony defect and prevents the humeral head from slipping out again during shoulder movement.
This technique is particularly useful in patients with moderate bone loss or high-risk profiles for recurrent dislocation, such as:
- Young male athletes
- Contact or collision sport athletes
- Patients with hyperlaxity or multiple prior dislocations
Outcomes and Evidence-Based Results
Studies have shown that standard arthroscopic Bankart repair alone has a recurrence rate of 15–25%, particularly in younger, high-demand athletes. When combined with the remplissage procedure, recurrence rates drop significantly.
-
Recent evidence supports the superiority of remplissage in high-risk patients:
- A large systematic review and meta-analysis found that isolated Bankart repair had significantly higher rates of recurrent dislocation (OR = 4.22) and revision surgeries (OR = 3.36) compared to Bankart plus remplissage, with no significant difference in shoulder range of motion1.
- A multicenter randomized controlled trial (RCT) demonstrated that remplissage significantly reduced both failure rates (8% vs. 22%) and recurrent instability (10% vs. 30%) over a 4-year follow-up2.
- Another meta-analysis concluded that remplissage plus Bankart is superior to Bankart alone in reducing redislocations and improving shoulder function in patients with engaging Hill-Sachs lesions3.
- In off-track lesions, a retrospective study confirmed that remplissage lowered redislocation risk, though it may result in minor loss of motion4.
- A long-term follow-up study (mean 8 years) of remplissage + Bankart reported only a 5.6% recurrence rate, with high patient satisfaction and preserved range of motion5.
- A large systematic review and meta-analysis found that isolated Bankart repair had significantly higher rates of recurrent dislocation (OR = 4.22) and revision surgeries (OR = 3.36) compared to Bankart plus remplissage, with no significant difference in shoulder range of motion1.
-
Procedure > Recurrence Rate
Bankart Repair Alone
15–25%
Bankart + Remplissage
5–10%
Bankart + Remplissage (athletes)
4–8%
Optimized Recovery: Beyond Surgery
Dr. Jazayeri's approach to recovery extends far beyond the operating room. He incorporates a comprehensive strategy to support healing, accelerate recovery, and reduce risk of reinjury.
-

Nutritional Optimization and Amino Acid Supplementation
To combat the catabolic stress response after surgery, Dr. Jazayeri implements a protocol of targeted amino acid supplementation designed to:
- Preserve lean muscle mass
- Support collagen synthesis
- Enhance tendon-to-bone healing
This nutritional optimization is especially important in athletes and active individuals aiming to return to high-performance levels.
- Preserve lean muscle mass
-

Sport-Specific & Digital Physical Therapy
Each rehabilitation plan is customized based on the sport, position, and physical demands of the patient. In addition, digital physical therapy tracking tools are used to monitor progress, ensure adherence, and allow real-time communication between patient, therapist, and surgical team.
-
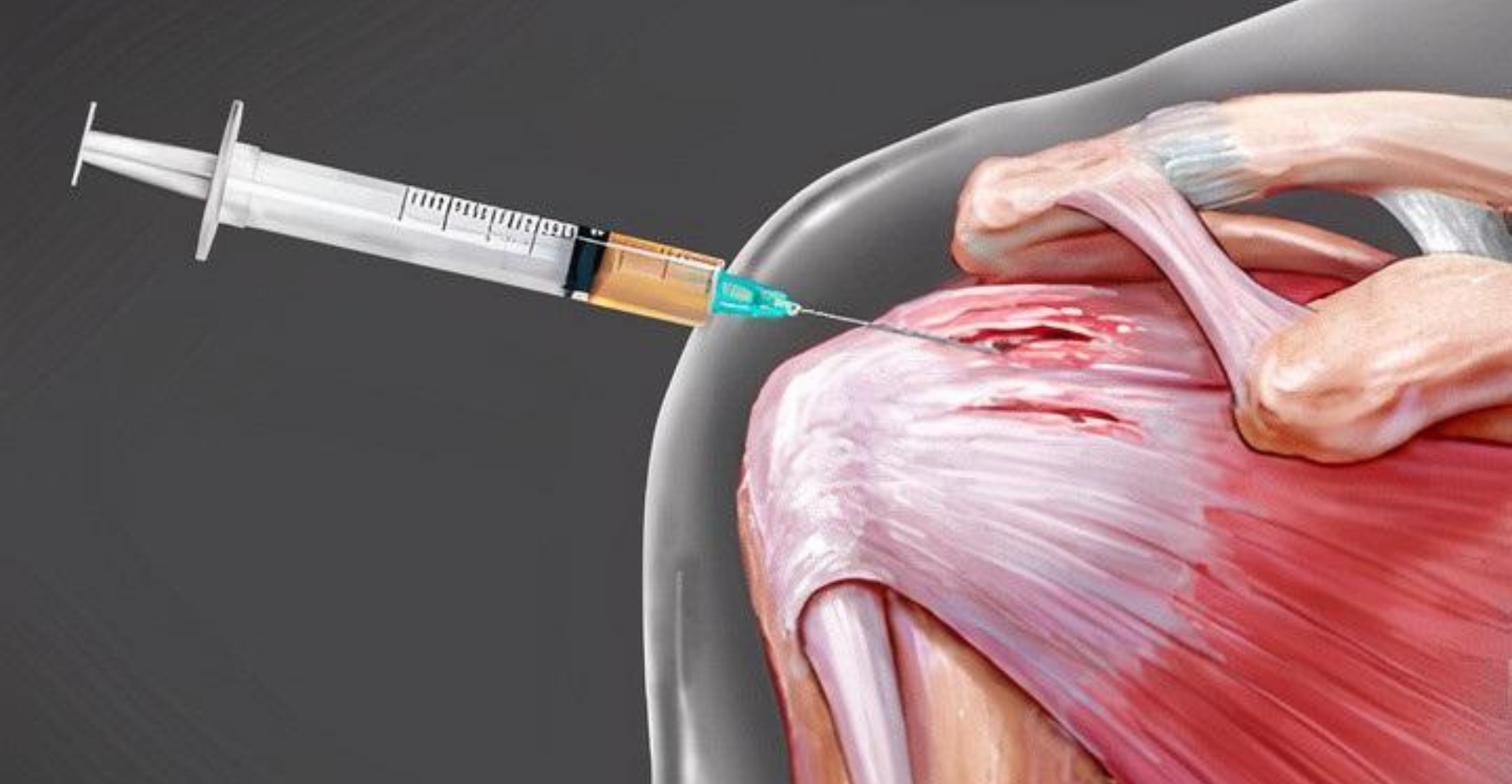
Orthobiologics to Support Healing
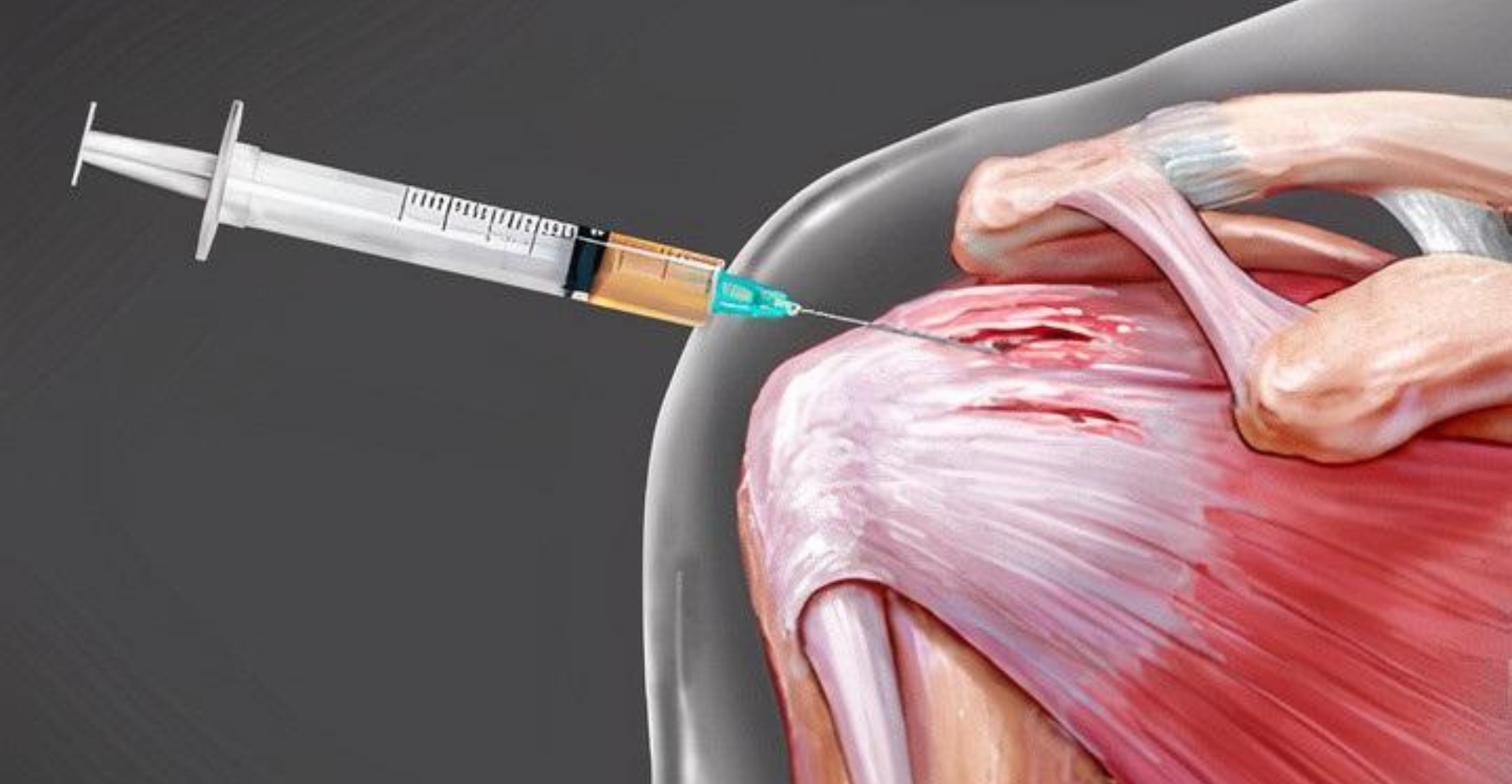
Dr. Jazayeri also offers select patients the option to incorporate orthobiologic augmentation, such as platelet-rich plasma (PRP) or bone marrow-derived products, which may help:
- Modulate inflammation
- Stimulate healing at the labrum and capsule
- Promote earlier return to activity
These adjunctive treatments are carefully selected and discussed based on the individual’s goals, tissue quality, and surgical findings.
- Modulate inflammation

Return to Sport:
Personalized Strategy for Athletes
A traumatic shoulder dislocation during the season can be devastating for an athlete. Dr. Jazayeri works closely with each patient to determine the best strategy, balancing:
- Risk of recurrence
- Timing within the competitive season
- Functional demands of the sport
- Long-term shoulder health
He develops personalized return-to-play protocols and leverages advanced surgical techniques, nutritional support, and modern rehabilitation strategies to help athletes return to sport with confidence.
Contact us
If you have questions or concerns, please don’t hesitate to ask Dr. Jazayeri or the care team: (855) 892-0919
Call nowClinical Research
References
1
Villarreal-Espinosa JA, et al. Remplissage vs. Bankart Alone: A Systematic Review and Meta-Analysis. J Shoulder Elbow Surg. 2024
2
Woodmass JM, et al. Multicenter RCT Comparing Bankart Repair With and Without Remplissage. Am J Sports Med. 2024.
3
Camus T, et al. Is Remplissage Superior to Bankart Repair Alone? Orthop J Sports Med. 2018.
4
Pandey V, et al. Remplissage in Off-Track Lesions: Reducing Redislocation Risk. J Shoulder Elbow Surg. 2020.